PAIN: Ergonomics How and Why
PAIN: Ergonomics How and Why By: Dr. Bob Niklewicz PT, DHSc, CEAS II “The Ergo Whisperer”
One of the primary reasons people seek out Ergonomics interventions at their work station is because they are experiencing PAIN. Those who are Ergo savvy, will make ergonomics changes to their work stations prophylactically to avoid pain. However, that might beg the question, does everyone understand How and Why Pain is experienced?
In this article I will go over some of the BASICS on How and Why Pain is experienced. This is not meant to be an all-inclusive dissertation on pain nor is it a diagnostic or treatment plan for pain. The intent is to provide a little enlightenment about a subject that may affect most people at some time in their lives. Hopefully this introduction to the realm of Pain Mechanisms and Healing will provide you with some enlightenment.
Introduction
Right off the bat, you have to understand that Pain is a normal part of life. If we did not have Pain, a person would not survive. Pain is a warning that there is something wrong and needs to be addressed.
Having occasional Pain is part of the human experience. However, it is not normal to have to “live” with Pain. From the ergonomics perspective, we may begin to experience pain in our soft tissues. Soft tissues include: muscles, tendons, ligaments, nerves and blood vessels. Pain in these tissues is generally classified as a Musculo-Skeletal Disorder (MSD).
In the study of Ergonomics, we know that the Primary Risk Factors for MSDs are: Posture, Repetition, Force, Contact Stress (think Direct Pressure) and Vibration. When tissue is stressed by those risk factors the soft tissues may start to fail or break down. When that occurs, the body tries to heal itself. Healing takes time. Avoiding the causative problem is necessary for healing too.
“GEE, it would be great not to have Pain?” is something that I have heard many times over the years as a Physical Therapist. I understand the desire to be pain-free, but in reality, if a person is truly pain-free, their life expectancy would not be very long.
There is a condition where a person is born without the ability to sense pain. They are truly pain-free. Sadly, these children die early as they break bones, get wounds, get burned, infections, bleed or have other traumas of which they are unaware. This condition is called “Congenital Insensitivity to Pain (CIP). In some cases, they are also unable to sweat and they suffer from hyperthermia. That is called, “Congenital Insensitivity to Pain with Anhidrosis” (CIPA).
Fortunately, the vast majority of us DO have an “Alarm System” called Pain. We also need to understand what is a serious problem and what is part of the progression of injury and healing. Towards that end, let’s look a little closer at the body’s sensory system and MSDs.
Pain and MSD’s
To give some perspective, there are approximately 400 individual nerves that travel about 45 miles through our body. Each of the nerves is very fragile. If you were able to touch one, it would feel much like a piece of boiled Vermicelli. It is soft, thin and easy to damage when stressed or compressed. Think about a road map showing roads going to thousands of locations. This is how the nerves are laid out and innervate the whole body.
Pain can occur from a sudden onset or a progressive injury over time. An example of a Sudden Onset Injury is the common “rolling your ankle or falling onto your wrist”. Accumulative Injuries can also occur over time. This is where the tissue is injured from constant repetitive and/or postural, submaximal forces. This condition is associated with an inflammatory response. NOTE: The risk factors for this type of injury may be familiar to you: Posture, Repetition, Force, Contact Stress and Vibration.
These risk factors can be further categorized into three mechanisms for injury that causes pain. They are: Mechanical, Thermal and Chemical sources.
Mechanical comes from something physical. This would be from movement/compression/pinching/ impact/tearing of a soft tissue. An example is a Carpal Tunnel injury where the Median Nerve is compressed by bad posture, force, repetition, contact stress and vibration at the wrist. (Does that sound familiar?)
The 2nd mechanism is Thermal. This is an injury from exposing tissue (mostly the skin) to excessive heat or cold that damages the tissue to different depths depending on the intensity and duration of exposure.
Chemical pain (sometimes called Stress chemicals) is the 3rd mechanism. This occurs when the tissue is exposed to an external chemical (extreme acid or base) and/or from chemical exposure released inside the body as a response to thermal or mechanical trauma. These chemicals are generally “histamines and cytokines” that are actually needed for initiating the healing process.
The 5 common signs of an injury are: Warmth (Calor), Swelling (Tumour), Redness (Rubor), Pain (Dolor), and Loss of Function (Functio laesa). Any of these signs may be more or less present than the others. In any event, your body doesn’t feel right and you begin to sense there is a problem. At this point the body’s alarm system (PAIN) goes off, you become aware and seek help.
The pain signals are sent to the brain where it is interpreted as pain and identifies where the pain is located. The intensity of the pain can be modulated by higher brain centers. The pain sensation may be reduced or increased by your emotional stress response. There may be a difference in pain sensation if you are calm and not anxious about the onset of the pain. In this case the intensity of the pain will be interpreted as being less severe. If you are quickly overwhelmed by the pain your perception of the level of pain may be greater than at other times.
If this alarm mechanism is ignored, the tissue can become HYPERSENSITIVE. If this occurs pain signals are sent to the brain with less provocation/stimulation and remain active for a longer period of time.
Key Facts & Function of Nerve Sensitivity
- When you develop pain, your nerves increase their sensitivity to protect you.
- A pain response is a normal occurrence in every person who is injured.
- The pain response is modified over time based on previous and ongoing injuries.
How it works
Throughout the body, all tissues have nerves endings called Receptors that provide information to the Brain. We have Joint Receptors that tell your brain what position your joints are in. Skin Receptors for sensing touch, temperature and for pain. (Your internal organs also have Receptors for pain as well. We will only be focusing on MSD’s.)
We also have nerves that go to healthy muscles that produce motion when we need or wish to move. There are also muscles that function automatically (as in breathing and pumping blood.) All of these amazing actions are performed by nerves for sensation and movement. Nerves begin in the Brain at specific areas. Many are involved in pain awareness. How and where in the brain the pain signal is perceived will determine how the experience will be processed, accepted and then acted upon. Figure 1 illustrates how the sensation from light touch is conveyed to the brain.
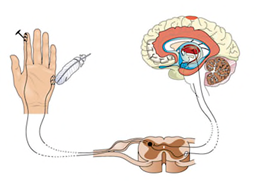
Figure 1. Feather touches the skin on hand. The signal goes up the arm to the spinal column that then conducts it to the Brain. This same process will determine if it is: sharp or dull pain, hot or cold, light touch or deep touch and/or vibration.
In an injury occurs to the muscle, tendon, or joint, pain nerve fibers are sent to the brain for interpretation of the severity and character of the stimulus. That in turn can result in you simply shaking your hand to get circulation going or even a quick withdrawal motion from a hot surface.
If there was a trauma to the tissue and the injury triggers an inflammatory response, such as in a sprain or strain, puncture wound or impact trauma, the healing cycle kicks in.
The Key Point here is that the receptors ONLY tell your brain that there is a problem. How your brain processes and analyzes this information will determine the extent and severity that the disability presents. The pain may be interpreted as not significant depending on what else is going on. e.g. You may not notice the pain from your sprained knee if you are running away from a fire or explosion.
Now what happens?
Pain presentation can be categorized by a timeline. Early on it is called an “Acute” injury. Conditions that have been present over a period of time are called “Chronic”.
This is important to understand. When tissue is injured, there is a very constant timeline for healing. This is delineated below in Figure 2.
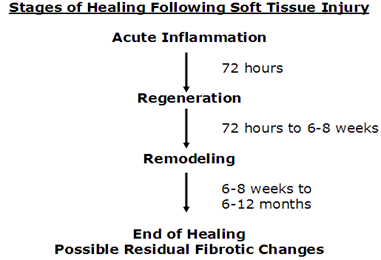
Figure 2 gives progressive windows for tissue healing. There is very little ability to speed up the healing process. However, it is VERY EASY to delay or prolong the healing process by returning to the offending activity too soon.
Proper first aid and self-care can keep you in this above window of time. Returning to full activity before healing is complete can cause the whole process to start all over again.
For a physical therapist like me, it is COMMON to have people become frustrated at this slow but normal process. Often, they may try and test the tissue too soon, only to reinjury it again. An injury that should be healing in 6-12 weeks is reinjured several times and may feel like the one injury has lasted for “Months”. In reality the person has had ONE injury but has suffered several “Reinjuries” that have lasted Months. The fear is that if the healing is frequently restarted from Reinjuries, the tissue may fail to heal altogether and become a Chronic problem.
Summary:
- Avoiding MSD’s is the best treatment for the problems they may cause.
- Seek medical advice and when you do so, PLEASE FOLLOW IT!!
- If injured, try to identify the offending activity and correct it immediately.
- If you cannot identify the cause, seek an ergonomics evaluation to help you identify it.
- Do NOT try to rush healing, it DOESN’T work!
- If you are referred to a P.T., be nice to them. Not all of us enjoy teaching you a lesson about Pain the hard way.
Watch for future articles on treatment options for MSD’s.


